More than 17 million Americans lost their Medicaid coverage in the past year, cutting them off from the government program that helps to cover medical costs for people already living on limited incomes.
The financial destabilization of that drastic drop in government support for low-income households fell disproportionately on people of color, a recent study found.
Throughout the COVID-19 pandemic, states received federal funding to maintain continuous Medicaid enrollment for individuals without needing to renew or provide additional information. The continuous enrollment period that automatically renewed participants concluded at the end of March 2023, giving states just over a year to solve the thorny question of “unwinding” Medicaid automation: How to identify those who remain eligible, those clearly ineligible and those whose eligibility is unclear without gathering more information.
Each state was free to approach the “unwinding” of that temporarily automated system however they chose. Some chose to use snail mail notifications that place the burden of proof on recipients, with mailing lists that often weren’t updated during the pandemic, inevitably removing some people from the program who in fact remain eligible. Few took the advised approach of using existing income tax data to answer the question without burdening low-income working families with paperwork or risking that a letter doesn’t reach the intended recipient.
The deadline to complete the “unwinding” process is the beginning of May 2024. The impact has already been massive: More than a third of all people who were receiving benefits from those programs as of March 2023 have been disenrolled through this “unwinding” nationwide.
A recent study published in the Journal of the American Medical Association (JAMA) Health Forum found those disenrollments to be racially inequitable. Black patients were over 10% more likely than White patients to be disenrolled, Hispanic patients nearly 20% more likely, while Native American and Alaskan Natives were more than twice as likely to lose coverage.
This may reflect the skew among states toward bureaucracy-heavy snail-mail solutions to unwinding. Although the JAMA study focused on the inequities themselves and not their potential causes, Kaiser Family Foundation data indicate that the vast majority of Medicaid disenrollments have been marked “procedural reasons.” A procedural disenrollment means that nobody actually figured out those enrollees should be kicked off Medicaid – they just didn’t get required paperwork from those households and summarily removed them from the program.
When Medicaid expansion began, many in the public health and community development sectors celebrated what it would mean for health and wealth outcomes in neighborhoods across the country. Beyond providing access to necessary medical services, it provided financial protection to families, created jobs and contributed to the overall well-being of communities. The initial rollout came with millions of dollars to support community engagement efforts in underrepresented neighborhoods, significantly reducing uninsurance rates in our nation’s most heavily redlined communities. These are the same communities that are disproportionately impacted by the failure of states to effectively engage them during the renewal process.
Medicaid disenrollment is not merely a statistical trend; it has profound implications for individuals and families. Studies have shown that Medicaid coverage can significantly reduce medical debt, with an average decrease of $1,140 per enrollee. Moreover, individuals enrolled in Medicaid see their credit scores improve significantly, saving them an average of $280 a year in reduced borrowing costs across the board – a subtle but significant boost to their financial stability. The financial shelter provided by Medicaid coverage also means enrollees are less likely to be evicted, underscoring the healthcare program’s role in preserving housing stability for vulnerable populations. That research predates the expansion of Medicaid in some states to cover housing costs for those most at risk.
The large-scale and racially inequitable disenrollment process scrutinized in the JAMA study is therefore worrying on a variety of levels. One of the most alarming aspects of the disenrollment process is its impact on individuals struggling with mental health or substance misuse comorbidities. Shockingly, those with these health issues were 50% more likely to lose Medicaid coverage in this “unwinding” of COVID-era policy than their counterparts without such conditions. This creates a critical gap in care for individuals with some of the highest mortality rates, leaving them without necessary medical support precisely when they need it most.
The consequences of all this extend beyond the individual, affecting the fabric of communities grappling with mental health challenges.
The loss of Medicaid coverage does not occur in isolation; it ripples through neighborhoods and familial networks, exacerbating existing disparities and hindering efforts toward economic mobility. As communities lose access to affordable healthcare, financial stability and mental health resources, the cycle of inequality perpetuates, further deepening existing divides. The impact on local economies is also notable, as the sudden reduction in healthcare services creates a ripple effect, leading to job losses and diminished community well-being.
The stark contrast between the shortcomings in community outreach for Medicaid renewals and successful vaccine outreach efforts highlights the importance of robust, community-driven engagement. While vaccine outreach strategies invested significant resources, engaged community partners and focused on local coordination, Medicaid renewals often relied on state-led, centralized approaches with limited community-based outreach focused on mailers and automated phone calls. In public policy terms, such techniques are effectively a choice by governments to err on the side of wrongly disenrolling some eligible households, rather than maximizing accuracy by using tax data and pursuing more robust and effective public outreach.
As the nation grapples with the consequences of Medicaid unwinding, it is crucial to address the racial disparities that have emerged. The unwinding process widened the gap in economic mobility, hindered community development and further undermined trust in our social safety net. To truly build resilient and thriving communities it is imperative to focus on inclusive, community-driven approaches that leave no one behind. The link between the automated top-down outreach that accompanied Medicaid unwinding and the troubling outcomes uncovered in the JAMA study underscores the importance of bringing community-based partners into the planning and implementation process to reduce these racial inequities.
Devin Thompson is NCRC’s Director of Health Equity and Impact.
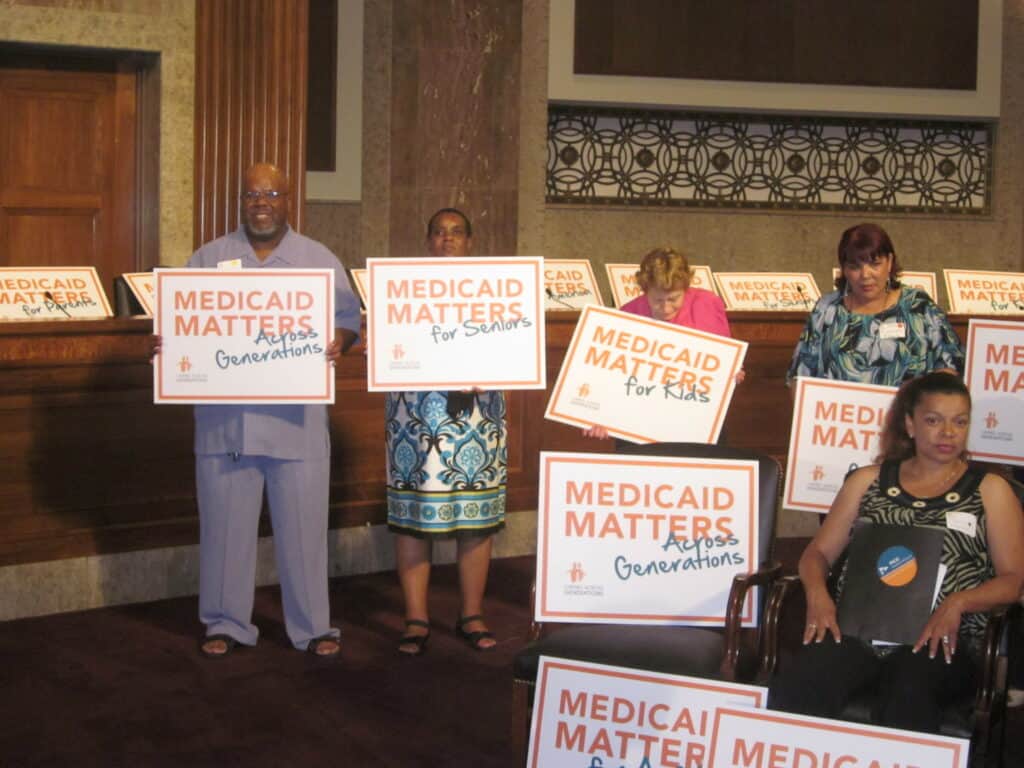
Photo via Jobs with Justice on Flickr.


Yes, I was dis enrolled. I have lupus. Many doctors and prescriptions. I am a widow, live alone and receive social security. I do not have enough money to pay the doctors or prescriptions. WHY.??? I am a sick person. What is going on????? Oh and I am white